A S Carlson (FBDO) MPhil. University of Johannesburg, Department of Optometry.
Much has been written about blue light and its adverse effects on the eye. The purpose of this article is not to re-invent the wheel, but to consider, or perhaps, reconsider the benefits and adverse effects of blue light on the eyes. Let’s first discuss sight, vision and then blue light before we get into the effectiveness and benefits of blue light control lenses.
Sight as a phenomenon can be broken down into different visual stimuli. There are conscious visual responses (image forming) and subconscious visual responses (non-image forming). Conscious vision is what is transferred to the visual cortex via the lateral geniculate body (LGB). Conscious visual responses can be classified in central vision, (object recognition), and peripheral vision (spatial vision). However, the peripheral retina, which are predominantly rods-covered are sensitive to both visual and non-visual stimuli including ambient light and are predominantly processed by sub-cortical brain centres. The retinal ganglion cells (RGC’s) can be classified in more than 11 types depending on the method of classification (Carcieri, 2003). Different classes of RGC’s transport different types of information, for example, contrast, movement, orientation, and ambient light to the brain. One class of retinal ganglion cell that play a particular role in ambient light processing is the intrinsically photosensitive Retinal Ganglion Cells (ipRGC). These sparsely situated cells are most sensitive to blue-light. They seem to exist principally to help differentiate between day and night thus modulating the sleep/wake cycles, known as circadian rhythms (Menaker, 2003).
Blue light is the radiation that ranges from about 400 nm to 500 nm. Wavelengths ranging from approximately 400 nm to 470 nm are believed to be harmful to the human eye. Recent research has found that light of this band triggers critical physiological responses, including pupil constriction and circadian rhythm synchronisation (Smick et al., 2013). Blue light of this wavelength cannot be absorbed by the cornea or crystalline lens and is transmitted directly to the retina. Excessive blue light of 400 – 470 nm may cause damage to the crystalline lens proteins and account for cataracts, accelerate the degeneration of retinal pigment cells and increase the acidification of retinal cells (Chen et al., 2015). In vitro studies done on animals have shown hazardous effects of blue light in ageing eyes through the accumulation of lipofuscin, which is commonly known as ‘the age pigment’ within the retinal pigment epithelium (RPE). Lipofuscin is stimulated by blue light and makes the retina and the fovea more vulnerable to high-energy blue-light radiation, leading to epithelial cell death (Smick et al., 2013; Menaker, 2003). As a result, lipofuscin accumulation has been implicated in the pathogenesis of age-related macular degeneration (ARMD) and intense auto-fluorescence is frequently observed in regions surrounding the leading edges of geographic atrophy lesions in the retina (Smick et al., 2013).
Other studies have shown that excessive exposure to harmful blue light induces the formation of toxic reactive oxygen species (ROS) that cause photochemical damage resulting in apoptosis of retinal cells. This leads to the worsening of severe ocular damage such as ARMD (Leung et al., 2018; Smick et al.,2013;). Apart from ARMD, blue light is also related to uveal melanoma as wavelengths of 400-500 nm, specifically in the 425 nm–475 nm range, can reach the posterior uveal tract with sufficient energy to cause destruction to the components of the eye, such as creating ROS in the mitochondria, resulting in cell dysfunction or cell death. Reactive oxygen species attacks many molecules within the eye. For example, ROS attacks polyunsaturated fatty acids, which form one of the major components of cell membranes. The large concentration of fatty acids in cell membranes in the retina makes the retina highly sensitive to oxidative stress. This stress may disrupt the membranous structures of the photo-receptor outer segments of the retina, causing incomplete phagocytosis and digestion of oxidised outer segments in the RPE which may result in the accumulation of the lipofuscin waste product and RPE cell granules (Smick et al., 2013). The exact mechanism by which blue light increases the proliferation of uveal melanoma cells is unknown, however, it is known that light of shorter wavelength provokes RPE cell death by ROS production. Blue-light therapy used for neonatal purposes, such as treating jaundice, increases the risk of developing dysplastic nevi in the eyes and skin, and is a further risk factor for melanoma. Therefore, it is imperative for eye protection to be worn to save the neonate from exposure to the lower-frequency blue light. Blue light is also a possible mechanism for tumorigenesis by inducing nuclear deoxyribonucleic acid (DNA) lesions due to the presence of lipofuscin. Blue light is not directly absorbed by the DNA but rather exerts its effect through a photochemical interaction with melanin. These biological effects coincide with UVA (ultraviolet A) wavelengths as they are both capable of producing ROS and causing melanocyte mutation. In addition, blue light also plays a role in neovascularisation, seen as a vital component of developing solid tumours such as uveal melanomas (Logan et al., 2015).
Studies suggest that retinal changes associated with age have a significant influence over the potential for photo damage. As the eye ages, light transmission and absorption changes, primarily owing to the gradual yellowing of the crystalline lens. As a result, the ageing lens transmits less visible light with a disproportionate drop in transmission of blue light due to the yellow discolouration of the lens. Early in life, blue light represents about 20% of the visible light received by the retina, dropping to approximately 14% at 50 years of age and to about 10% at 70 years. There is a gradual decrease of retinal exposure to blue light with ageing and the natural defences and repair mechanisms at the retina become less effective, therefore, the ageing retina remains susceptible to photochemical damage from the harmful blue light even as its level of exposure drops. The potential connection between the blue-light photo toxicity and retinal diseases such as ARMD suggests that reducing exposure to the harmful blue light would be beneficial for long-term ocular health (Smick et al., 2013).
Not all blue light is destructive as blue light of wavelengths approximately 470 nm – 500 nm is essential for normal visual functions and is believed to have effects on our psychological health and increases our feelings of well-being (Leung et al., 2018). Intrinsically photosensitive retinal ganglion cells are believed to exist along with the rods and cones. They form a photoreceptive network broadly within the inner retina, unlike the cone cells which are concentrated at the fovea. These cells are believed to contain melanopsin which is a photo pigment. The ipRGC responds to light in the chrono-biological band which regulates many non-visual physiological functions in the human body including circadian regulation, melatonin regulation, pupillary light reflex, cognitive performance, mood, locomotor activity, memory and body temperature (Smick et al., 2013).
Blue light therefore plays an essential role in our daily lives. Filtering out the entire blue spectrum to reduce the blue-light hazard may interfere with the physiological functions driven by the reaction between ipRGCs and light in the chrono-biological band. Other studies have shown that blocking blue light at 470 nm could disrupt the sustained phase of the pupil constriction (Smick et al., 2013). Blue light is important because it helps the short-wavelength cone photoreceptors of the eye in colour discrimination and possibly night vision (Leung et al., 2018). These photoreceptors have maximum sensitivity under blue stimulation (Burkhart and Phelps, 2009). Several studies have shown that the circadian cycle is primarily dependent on blue light, suggesting that its stimulation to the brain regulates the circadian cycle by inhibiting melatonin secretion (Burkhart and Phelps, 2009). These wavelengths range between approximately 380 and 500 nm. Nowadays, the human eye is potentially exposed to excessive amounts of the harmful, shorter wavelength blue light through digital devices such as tablets, computers, cellular phones, LED bulbs and all other artificial light sources emitting this type of light (Lawrenson et al., 2017). However, the level of blue-light exposure from computer screens and other LED-emitting devices is less than the level of blue light exposure from daily light (Leung et al., 2018). Nevertheless, blue light from these digital devices suppresses melatonin by about 23%. The use of longer wavelength light definitely has less influence than that of ‘blue light’ and is recommended for use at night (Marshall, 2017). Avoiding blue light for about 2 h – 3 h before bed helps the body prepare better for improved sleep. Ayaki et al., (2017) suggests that the reduction of blue light also lessens eye fatigue and dry eye symptoms. Apart from minimising blue light, the bright light that we are exposed to during the day should be maximised (Marshall, 2017). The exposure to artificial light at night not only influences sleeping patterns, but also appear to cause weight gain, depression, cancer, and heart disease (Marshall, 2017). The American Medical Association issued a statement claiming that bright light emitting diodes (LED) lights are causative components of chronic disease risks. The specialised cells in the retina respond to the shorter wavelength light that affects the circadian rhythms. As these cells are stimulated, the brain is awoken, decreasing melatonin levels, and driving out drowsiness, due to hormones such as cortisol (stress) and ghrelin (hunger) being produced.
The Circadian Rhythm is much more than just a sleep-wake cycle. A lot of cells have their own internal clock. The endothelium in the blood vessels for example, has an inherent relaxation and contraction cycle, more or less based on a 24-hour cycle. Circadian Rhythm is more than just hormones and nerves. The circadian impulse influences the genetic machinery of targeting cells, which then produces proteins and enzymes that makes the organ function (Hater, 2002). Dysfunctional circadian rhythm has been correlated to heart disease, worsening with metabolic syndrome, and breast and colon cancer (Smick et al., 2013).
For metabolism to work optimally the circadian rhythms of the lipid, glucose and cell function should be in sync. According Spiegel et al., (2009) shift-work and sleep deprivation are known to dampen rhythms in the growth hormone and melatonin, reduce insulin sensitivity and elevate circulating cortisol levels. These changes favour weight gain, obesity, and development of the metabolic syndrome (Vimont, 2017). The goal of treatment should thus be to reset or synchronize the circadian rhythm (Lawrenson et al., 2017).
Vignozzi and Maggi, (2020) found a correlation between erectile dysfunction and men with shift work sleep disorder. The reduced erectile function is probably due to a generalize asynchrony of the vascular and hormonal systems, but importantly also due to the asynchrony of the pineal-melatonin-testosterone function. Bossini et al., (2013) found in a randomized controlled trial that within two weeks’ light therapy improves sexual satisfaction about 3 times compared to a placebo.
Circadian Rhythm and Cognitive Function
Vandewalle, Maquet, & Dijk, (2009) has done research on specifically ambient light and cognitive performance by asking subjects to perform auditory tasks while being exposed to monochromatic light. They also did positron emission tomography (PET) of subjects in order to identify the brain structures involved. They found that behavioural performance was optimal for light with wavelengths of 460nm (blue light, melanopsin peak sensitivity). There was a correlation between intensity and duration of light exposure at night and day. Ambient light would activate brain centres for the duration of exposure, but bright light will affect the brain sectors for several minutes after the stimulus were stopped. The amygdala (limbic or emotional brain), hippocampus (memory) and the superior parietal cortex were affected. However, they believe the brain centres involved will change depending on the tasks that were involved.
Lately the idea that blue light blockers might improve ADHD symptoms and sleeping function is circulating in public. From the above evidence one can argue that blue blocking lenses reduce the excitatory light input and hence “causes sleep or relaxation”. It is easy to fall in a trap where one thinks it is OK to use red filters to improve sleep function and blue filters to increase excitement. In truth, both red and blue light will cause excitement, but blue light causes more excitement at the same intensity than red light. We may therefore doubt whether one can truly say that by changing the background illumination on your phone or computer, would really be beneficial for sleeping. No-light, (darkness) is still better than red light. One also has to consider that the suprachiasmatic nucleus (SCN) receives input from other brain centrums’ than the retina, which will also influence mental activity. One should therefore be clear that blue blocking lenses might be part of the solution to reduce sleeplessness and anxiety or alternatively that exposure to blue light might increase awareness and cognitive function, but will most likely not solve all problems.
As Optometrists we have be inundated with the sympathetic and parasympathetic systems. One’s gut might tell you that your sympathetic system might be more active during the day and your parasympathetic system more active at night, and that the SCN regulates the shift between the two. Unfortunately, it is not so simple. Consider bladder function. The sympathetic system increases the volume the bladder can handle, but also keep the urinary sphincter muscle closed. The role of the SCN is not necessary to change the shift from sympathetic to parasympathetic, but to keep the urinary system closed at night, so one can sleep in peace. With light therapy or light blocking filters, one can modulate or tone down the neurological response but it is also more a shift of the circadian rhythm toward the beginning or end of the wake-sleep cycle. With a partial blue control filter one can perhaps change the daytime amplitude of the wake cycle downwards and maybe decrease the length of the daytime cycle. However, it is still worth to consider blue-blocking lenses or light exposure as a therapy. One way to keep drivers awake at night might be to try and expose them to strong blue light before undertaking long trips at night.
Due to the hormonal effect and the possible permanent changes light can have on the brain of children, especially as far as sexual development is concerned, one should maybe think twice before jumping on the blue light bandwagon.
Blue Light and Retinal Dopamine
The ipRGC also project to the inner-retina, especially to dopamine secreting (GABAergic) amacrine cells. However, it is not clear what exactly the relationship between ipRGC and retinal dopamine levels are as the rod-photoreceptors are mainly responsible for retinal
dopamine production (Munteanu, et al., 2018). One of the consequences of diabetes (in mice) is a reduction of retinal dopamine, which in turn leads to a loss in contrast sensitivity and acuity (Aung, et al., 2014). In mice retinal dopamine levels can disappear within 6 weeks after the induction of diabetes, and the loss of acuity and contrast sensitivity happens before vascular changes are noted. The retinal dopamine cells develop in the early stages of development, and experiments with mice has indicated that if interrupted in the development phase, the deficiency persist until adulthood and presumably until death. According to Zou et al., (2017) retinal dopamine has an antagonistic effect on retinal growth. It is, however, not a simple relationship but it is clear that bright peripheral light decreases retinal growth in chickens. What is perhaps positive is that bright light under laboratory conditions has shown a more consistent effect than outdoor light. This most likely because outdoor light levels are subjected to change due to cloud coverage etc. It’s also not clear whether the light source or the focal length of the light rays are important. It appears that at least in diabetics, a reduced VA can be a result of depleted retinal dopamine, which in turn can be worsened by blue light filters. Ironically, with all the blue-blocking marketing that is primarily focused on the dangers of blue light, the concerned optometrist might prescribe a blue blocker precisely when he or she shouldn’t. Also, is it important to note that blue light blockers might decrease the dopamine concentration in the retina, and hence decrease the retinal growth stopper. It should be self-evident that blue light blockers are contraindicated for young emmetropes, and myopes. At the same time, it might be indicated for young hyperopes.
Blue light and Anterior Chamber, and Intra Ocular Lens – Glaucoma.
The American Academy of Ophthalmology published an article to the public denouncing the idea that blue light from computer screens are damaging to the eyes. However, it might be that blue light damages the mitochondria in the RGCs that are already compromised by other pathological stress, e.g. glaucoma, thus worsening glaucoma (Bullough, 2017). Dopamine has been shown to reduce the intra ocular pressure, but it is highly unlikely that dopamine from the posterior pole – secreted due to blue light exposure – might reach the ciliary body, and anterior chamber. Whether ipRGC and amacrine cells near the ora-serrata might secrete enough dopamine to cause a reduction in IOP is not known. Prescribing blue blocking lenses might therefore be indicated for patients who already suffer from glaucoma. However, as incredible as it might sound, there is another reason why blue blocking lenses might be considered – melatonin production in the anterior chamber. Lledo et al., (2019) did experiments on mice and found that continuous exposure to monochromatic yellow light reduced IOP up to 40%. The non-pigment epithelium of the ciliary body processes contains melatonin receptors. Melatonin is produced at night and secreted into the aqueous, diffuse towards the ciliary body where it inhibits aqueous production, which in turn leads to a reduction at IOP. Light including blue light stimulates melanopsin, which inhibits melatonin production, which increases IOP. Blue light filters, including yellow lenses inhibits the inhibition of melatonin-production by melanopsin, which leads to a decrease in IOP.
Clinically, it’s important to note that diabetics may suffer from melatonin dysfunction, hence blue light filters might be suitable for diabetics as well as a way to reduce the dosage of glaucoma medication, especially where side effects are a problem.
A comparative study was done by Carlson (2019) on the transmission of blue light through ten different blue control lenses. Seven lenses had blue control reflecting coatings while three had in-mass absorption properties. The blue reflective coatings were Preventia (Essilor), Shamir Glacier Blue and Blue Shield (Shamir), Hoya Blue control (Hoya), the MR Blue Coat, I Relief from BBGR and the Zeiss Drive. The In- mass lenses were Kodak, Shamir Blue Zero and the GKB lens.
Figure 1 shows the Transmission of radiation through the ten lenses between 350 – 500 nm. Table 1 shows the percentage transmission of blue light between 400 – 500 nm, the percentage loss due to reflection or absorption as well as percentage transmission and reflection or absorption between 400-470 nm and 470–500 nm respectively through each lens. An Achromatic lens that is an ordinary ARC lens with no blue control coatings is the control lens.
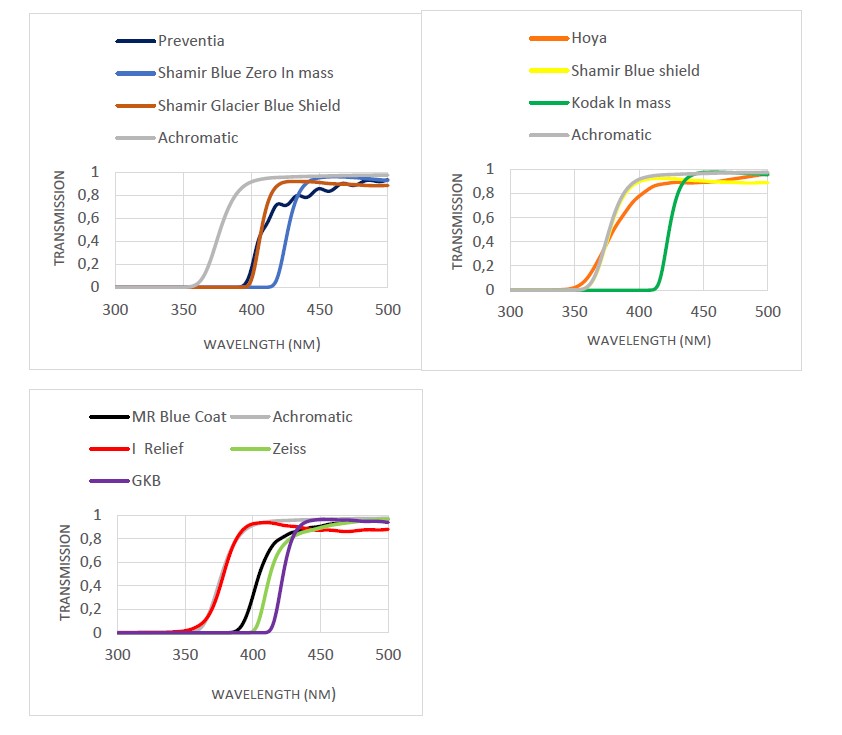
Figure 1. Transmission curves for the 10 blue control lenses. The Achromatic anti-reflection coating lens is the control lens.
Figure 1. Transmission curves for the 10 blue control lenses. The Achromatic anti-reflection coating lens is the control lens.
For wavelengths 400-500 nm the Hoya, I Relief and Blue Shield only reflects 10% of blue light while the MR Blue and Glacier reflect 15 and 17% respectively. The Zeiss Drive and Preventia reflect the most, 21 and 22% respectively. The in-mass lenses, the GKB (26%), Kodak (27%) and Shamir in-mass (31%) absorb the most. The Achromatic control lens reflects only 4% across the blue region of the spectrum.
Table 1. Table showing the percentage transmission (%) and reflection of wavelengths (nm) for blue light. The numbers in the Table represent percentages.
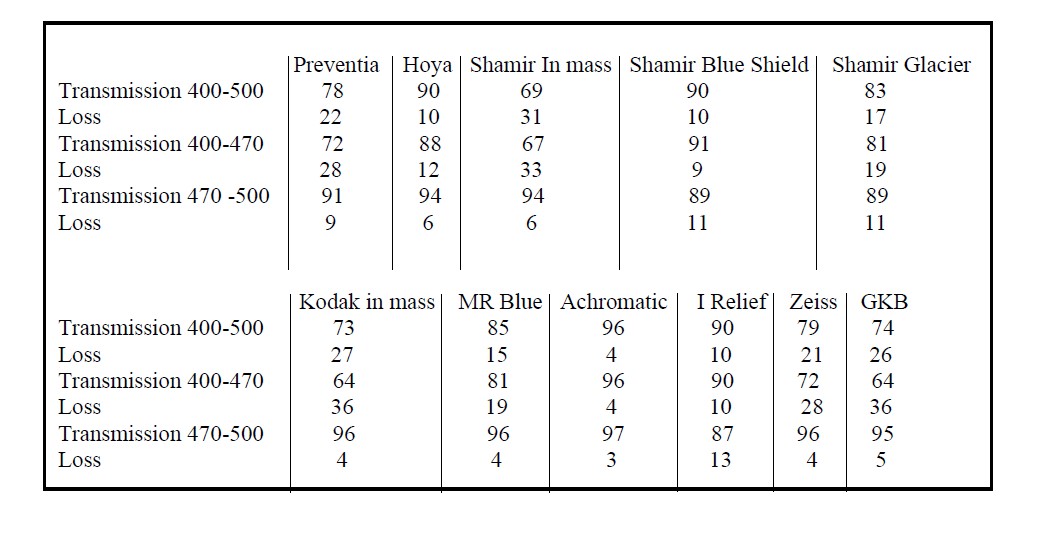
For wavelengths 400-470 (bad blue light), the Blue Shield reflects 9%, the I relief 10%, and the Hoya 12% while both the MR Blue and Glacier reflects 19%. The Zeiss Drive and Preventia both reflect the most, 28%. The In-mass lenses, the GKB (36%), Kodak (36%) and Shamir In-mass (33%) absorb the most. The Achromatic control lens reflects only 4%.
For wavelengths 470-500 nm, the Kodak in mass, MR Blue and Zeiss all reflect 4%, the GKB 5%, the Hoya and Shamir in-mass 6%, Preventia 9%, the Blue Shield and Glacier 11% and then the I relief 13%. The Achromatic control lens reflects only 3%.
The in-mass absorbing lenses appear to cut out more of the shorter wavelengths when compared to the reflective coatings. There does not appear to be any consistency amongst reflection properties for the shorter blue wavelengths.
Discussion
A study was done by Mainster et al., (2022) that ambient environmental light exposure causes photo-toxicity to the retina, leading to age-related macular degeneration (AMD). They analysed clinical, epidemiological, and biophysical data regarding blue-filtering optical chromophores. They found that large epidemiological studies show that blue-blocking intraocular lenses (IOLs) do not decrease AMD risk or progression. Blue-filtering lenses cannot reduce disability glare because image and glare illumination are decreased in the same proportion. Blue light essential for optimal rod and retinal ganglion photoreception is decreased by the progressive age-related crystalline lens yellowing, pupillary miosis and rod and retinal ganglion photoreceptor degeneration. Healthful daily environmental blue light exposure decreases in older adults, especially women. Blue light is important in dim environments where inadequate illumination increases risk of falls and associated morbidities.
They feel that blue-light-hazard is misused as a marketing strategy to alarm people into using spectacles and IOLs that restrict blue light. Blue light loss is permanent for pseudophakes with blue-blocking IOLs. Blue-light-hazard misrepresentation flourishes despite absence of proof that environmental light exposure or cataract surgery causes AMD or that IOL chromophores provide clinical protection. Blue-filtering chromophores suppress blue light critical for good mental and physical health and for optimal scotopic and mesopic vision.
There is limited literature on the impact of blue-blocking lenses on visual function and of the few studies found contradictory findings have been reported. Leung et al., (2017) investigated the effect of blue-blocker spectacle lenses on contrast and colour perception assessed using clinical tests and noted that there were no significant changes in these visual functions. The results by Leung et al., (2017) agree with a review article on blue-blocking intraocular lenses that also noted no significant changes in colour vision or contrast sensitivity (in mesopic and photopic conditions) in studies involving patients wearing blue-blocking intraocular lenses or ultraviolet light-blocking intraocular lenses (Cuthbertson et al., 2009). In contrast, Werner (2005) noted that blue-blocking intraocular lenses reduced contrast sensitivity in scotopic conditions. A systematic review reported that there are concerns over the use of blue-blocking spectacle lenses on some aspects of visual function including contrast sensitivity and colour vision (Lawrenson et al., 2017). In addition, the systematic review also concluded that there is insufficient high-quality evidence in the literature to support the use of blue-blocking ophthalmic spectacle lenses for reducing eye fatigue, protecting retinal health, and improving visual performance and sleep quality (Lawrenson et al., 2017).
Judging from the conflicting results from the different researchers, are we, as clinicians relying too much from information from the manufacture’s marketing divisions and consultants. If one is to read white paper literature, some researchers and authors appear to be from the R&D departments of those companies and may appear to have invested interests in the company. This is not to say that all the information is incorrect or not true. Maybe more investigating in the research is needed. As one says, prevention is better cure. But this may not always be the case.
It appears that the typical optometrist prescribes blue control lenses without considering the adverse effects. However, in the big scheme of things there is a place for blue light control, but that it is in effect not only the prescription of blue light filters that might have clinical importance but also the prescription of monochromatic light sources when reading or aiding in behaviour. One has to remember that while taking away blue light out of the spectrum, there is also in some cases a need to add blue light to the spectrum. It is rather difficult and give a more professional guideline on when and when not to prescribe blue light filters, but especially with the circadian aspect, a lot more research is needed.
References
Aung, M., Park, H., Han, M, Obertone, T., Abey, JFA. (2014). Dopamine Deficiency Contributes to Early Visual Dysfunction in a Rodent Model of Type 1 Diabetes. Journal of Neuroscience, 34(3): 726–736, https://www.ncbi.nl.
Ayaki, M., Hattori, A., Maruyama, Y., Tsubota, K., Negishi, K (2017). Large-scale integration in tablet screens for blue-light reduction with optimized color: The effects on sleep, sleepiness, and ocular parameters. Cogent Biol [serial online].[cited 2018 June 27] 3(1). https://doi.org/10.1080/23312025.2017.1294550.
Bechtold, D., Gibbs, J., & ASI, L. (2010). Circadian dysfunction in disease. Trends in Pharmacological Sciences, Vol 31(5), 191 – 198.
https://www.sciencedirect.com/science/article/abs/pii/S0165614710000039.
Bossini, L., Caterini, C., K. D., Casolaro, I., Roggi, M., Di Violo, S.. Gagiolini, A (2013 ). Light Therapy as a treatment for sexual dysfunctions – beyond a pilot study. Psychiatr Pol, Noc-Dec;47 (6):1113-22.
Burkhart, K., Phelps, JR (2009). Amber lenses to block blue light and improve sleep. A randomized trial. Chronobi Int J [serial online].[cited 2018 Feb 18] 26(8):1602–1612. Available from https://www.ncbi.nlm.nih.gov/pubmed/20030543.
Carcieri, SM., JA (2003 ). Classification of Retinal Ganglion Cells: A Statistical Approach. Journal of Neuro-Physiology, Sept 1, https://doi.org/10.1152/jn.00127.2003.
Carlson, AS (2019). A comparison of blue-light transmissions through blue-control lenses. Afr Vision Eye Health. 2019;78(1), a497. https://doi. org/10.4102/aveh.v78i1.497
Chen, D., Huang K, Lee S., Wang, J (2016). Blue light blocking lenses measuring device. Procedia Eng. 140:17–29. https://doi.org/10.1016/j.proeng.2015.10.150
Hattar, S., Liao, HW., Takao, M., Berson, DM., Yau, KW (2002). Melanopsin-containing retinal ganglion cells: Architecture, projections, and intrinsic photosensitivity. Science [serial online] [cited 2018 Mar 20] 295:1065–1070. Available from https:// www.ncbi.nlm.nih.gov/pubmed/11834834.
Lawrenson, GJ., Hull, CC., Downie, LE (2017.) The effect of blue-light blocking spectacle lenses on visual performance, macular health and the sleep-wake cycle: A systemic review of the literature. Ophthal Physiol Opt [serial online][cited 2018 Feb 18] 37(6):644–654. Available from https://www.ncbi.nlm.nih.gov/ pubmed/29044670.
Leung, TW., Li, RW., Kee, C (2017). Blue-light filtering spectacle lenses. Optical and clinical performances. PLoS One [serial online].[cited 2018 Feb 15]. Available from http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0169114.
Lledó, V. E., Alkozi, H. A., & J, P. (2019). Yellow filter effect on melatonin secretion in the eye: Role in IOP regulation. Current Eye Research, https://doi.org/10.1080/02713683.2019.1570276
Logan, P., Bernabeu, M., Ferreira, A., Burnier, MN (2015). Evidence for the role of blue light in the development of uveal melanoma. Journal of Ophthalmology [serial online]. [cited 2018 June 27]. https://doi.org/10.1155/2015/386986
Marshall, L (2017). Is blue light bad for your health? [homepage on the Internet]. [cited 2018 June 26]. Available from https://www.webmd.com/sleep-disorders/ news/20170619/is-blue-light-bad-for-your-health.
Mainster, M., Findl, O., Burkhard Dick, H., et al.,(2022). The Blue Light Hazard Versus Blue Light Hype. American Journal of Ophthalmology. Vol. 240, p51-57. Published:February 24, 2022DOI:https://doi.org/10.1016/j.ajo.2022.02.016
Menaker, M (2003). Circadian rhythms. Circadian photoreception. Science. Jan 10;299(5604):213- 4. doi: 10.1126/science.1081112.
Munteanu, T, Noronha, K., Leung, A., Pan, S., Lucas, JA & Schmidt, T (2018). Light-dependent pathways for dopaminergic amacrine cell development and function. eLife, 7:e39866 DOI: 10.7554/eLife.39866;
Smick, K., Villette, T., Boulton, ME., et al. (2013). Blue light hazard: New knowledge, new approaches to maintain ocular health. Essilor: Report of a Roundtable [homepage on the Internet]. [cited 2018 Aug 09] 37–47. Available from http://www. pointsdevue.com/sites/default/files/uv-bluelight-e-book.pdf.
Spiegel, K., Tasali, E., Leproult, R., & Van Cauter, E (2009, June). Effects of poor and short sleep on glucose metabolism and obesity risk. Nature Reviews Endocrinology. 5, 253–261;doi:10.1038/nrendo.2009.23.
Vandewalle, G., Maquet, P., & Dijk, D.-J. (2009). Light as a modulator of cognitive brain Function.
Trends in Cognitive Sciences Vol.13 No.10, 429 – 438 doi: 10.1016/j.tics.2009.07.004.
Vignozzi, L., & Maggie, M (2020). Circadian rhythm and erectile function: is there a penile clock? Nature Reviews. Urology. Nov;17(11), 603-604. doi: 10.1038/s41585-020-00376-7. PMID:32943773
Vimont, C (2017). Should you be worried about blue light? [homepage on the Internet]. 2017 [cited 2018 June 30]. Available from https://www.aao.org/eye-health/tips-prevention/should-you-be-worried-about-blue-light.
Werner, JS (2005). Night vision in the elderly: consequences for seeing through a “blue-filtering” intraocular lens. British Journal of Ophthalmology, 89, 1518-1521.
Zhou, X., Pardue, M., Luvone, P, & Qu, J (2017). Dopamine signalling and myopia development: What are the key challenges. Progress in Retinal and Eye Research, doi:
10.1016/j.preteyeres.2017.06.003.