Bart Johnson, Brian Pall, O.D., M.S., F.A.A.O., and Charles W. Scales, Ph.D
AN INNOVATIVE NEW CONTACT LENS DESIGNED
TO WORK WITH THE TEAR FILM
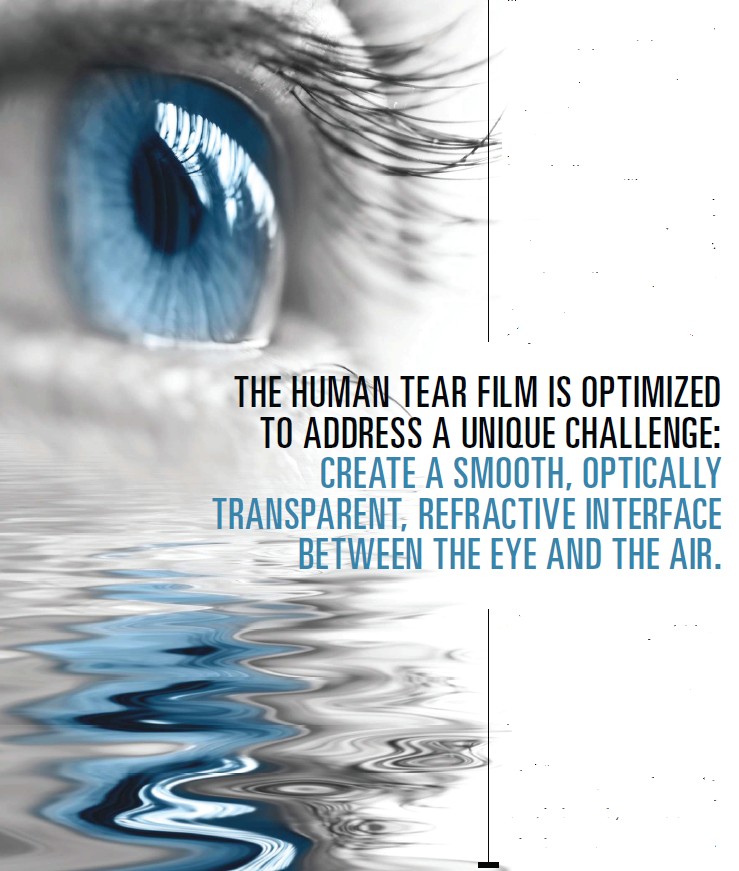
TEARS ARE vital to maintain a healthy ocular surface and an optically clear entrance to the eye. Without them, we would not have the sharp retinal image that allows us to see the world and each other clearly. Tears are rich and complex, and that richness is necessary for their efficacy.
Water alone could not nourish and protect the delicate corneal and conjunctival epithelia, nor give us the clear, stable vision we experience daily. The human tear film is optimized to address a unique additional challenge: create a smooth, optically transparent, refractive interface between the hydrophilic environment of the eye and the
hydrophobic external environment of the air.
This interface is stabilized through synergistic interactions of hydrophilic, amphiphilic, and lipophilic tear film components, including ocular mucins, proteins, and lipids. These components work in concert to continuously lubricate, moisturize, smooth, oxygenate, eliminate waste and protect the ocular surface during and between blink cycles.
A COMPLEX STRUCTURE
The old picture of the tear film consisted of a simple three-layer — mucin, aqueous, and lipid — structure. Recent research has revealed it to be much more complex, with more than 18 known mucins, 491 proteins (identified so far) and at least 153 lipid types — all of which interact to provide structural integrity to the tear film while also performing their individual functions.1,2,3 And each of the three major components of the tear film is itself multifunctional and complex in makeup.
Functions of the Tear Film Mucins
• Anchor and stabilize the tear .lm
• Protect ocular surface from abrasion through formation
of the glycocalyx
• Lubricate cell surfaces so corneal epithelium doesn’t
stick to tarsal conjunctiva
• Reduce shear stress during blink
 The base layer of the tear film is comprised of tear film mucins, which extend from inside the epithelial cells, through the hydrophobic cell membrane, to the outside of the cell. Called the glycocalyx, these high molecular weight mucins are bound to the cornea on one end but have hydrophilic tails that extend into and hold the aqueous to the cell surface (Figure 1, ).1
The base layer of the tear film is comprised of tear film mucins, which extend from inside the epithelial cells, through the hydrophobic cell membrane, to the outside of the cell. Called the glycocalyx, these high molecular weight mucins are bound to the cornea on one end but have hydrophilic tails that extend into and hold the aqueous to the cell surface (Figure 1, ).1
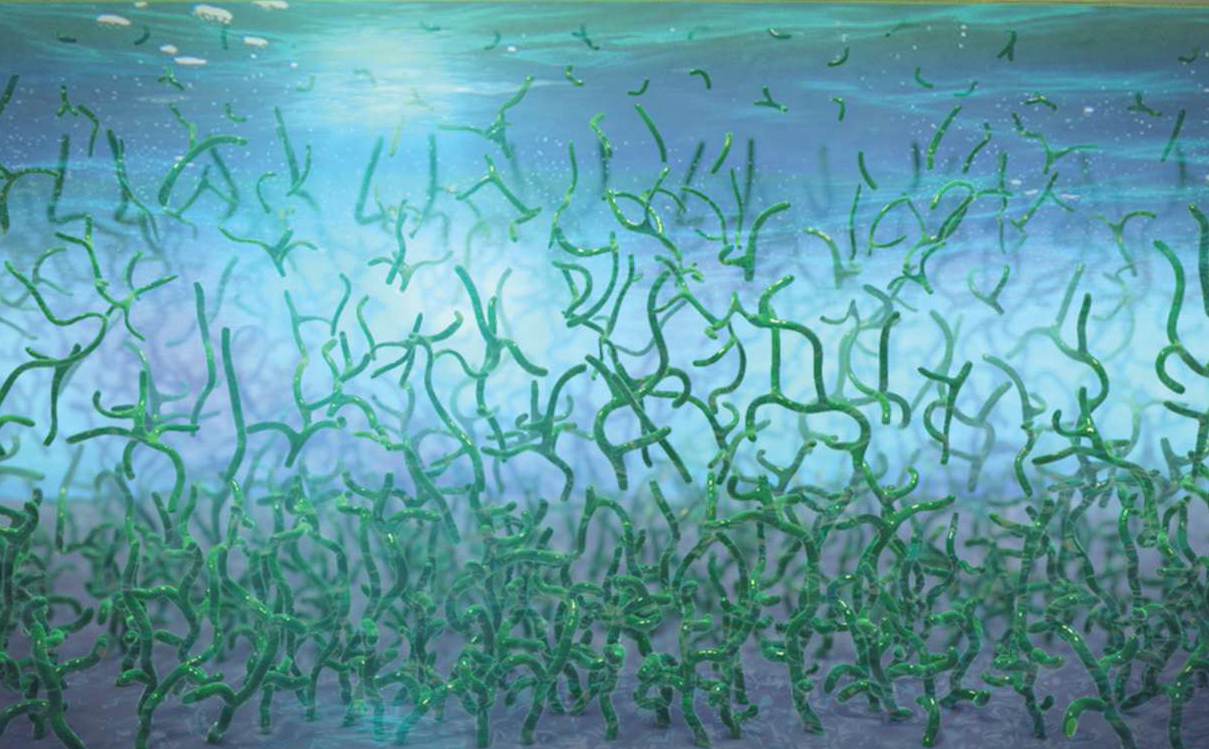
Figure 1: High molecular weight mucins are bound to the cornea on one end but have hydrophilic tails that extend into and hold the aqueous to the cell surface. Because cell membranes are largely hydrophobic, without these mucins, tears would run off the corneal surface. At the same time, the mucins act as a disadhesive so the corneal epithelium doesn’t stick to the tarsal conjunctiva.
Because cell membranes are largely hydrophobic, without the mucin glycocalyx, tears could run off the corneal surface like water off a teflon frying pan. (See “Functions of the Tear Film Mucins,” At the same time, the mucins act as a disadhesive so the corneal epithelium doesn’t stick to the tarsal conjunctiva.
Other mucins float freely in the aqueous compartment, which functions to clean, protect and transport nutrients and oxygen to the cornea.4 Much more than water, the aqueous contains large and small chemical entities —including environmental debris that will be disposed of through tear drainage.3
Above the aqueous is the lipid layer. Once considered a simple barrier to prevent evaporation, it is at least a two-layer structure, with polar lipids at the aqueous/lipid interface and a thicker layer of nonpolar lipids situated above the polar lipids and facing the air.5
The lipid layer aids in lubrication prevents loss of aqueous and helps maintain a smooth optical surface. Without the amphiphilic polar phospholipid interface, though, nonpolar lipids would spread poorly over the aqueous, creating a less stable lipid layer and leading to more rapid tear film break-up5
IMPACT OF A CONTACT LENS
In healthy eyes, tear film components work in harmony, When the tear film is compromised, this system can break
down, leading to dryness and discomfort, corneal staining and conjunctival redness and vision disturbances
What’s more, the changing environments that people experience daily, as well as the intense demands we
make on our eyes, all may affect optical performance and comfort.
A contact lens changes the ocular surface environment dramatically. On the eye, a contact lens “splits” the tear film, trapping the vital mucin layer behind the lens, dramatically reducing the volume of aqueous, and disrupting the lipid layer.7
A thinner pre-lens tear film layer increases evaporation and shortens tear film break-up time, which can impact vision.8
Ideally, a contact lens would mimic the tear film. To do that electively requires a lens with tear-like properties that can interact with and support not just its water component but the full range of tear film constituents: mucins, aqueous and lipids.
TEAR-INFUSED DESIGN
To meet this challenge, Johnson & Johnson Vision Care, Inc., has introduced ACUVUE OASYS Brand Contact Lenses 1-Day with
HydraLuxe Technology with a tear infused design.
These new lenses are comprised of an enhanced network of tearlike molecules plus highly breathable hydrated silicone that integrates with the patient’s own tear film each day(Figure 2), and leverages all the benefits of daily disposability as well. This network of tear-like molecules is uniform throughout the lens, not simply a coating, and works consistently all day as opposed to having to be blink released. Because the natural tear film is a complex system, the lenses are designed to work with the key tear film components (not just water) to lubricate and moisturize the lens and support the tear film throughout the day. (See “Tear-Infused Design,”)
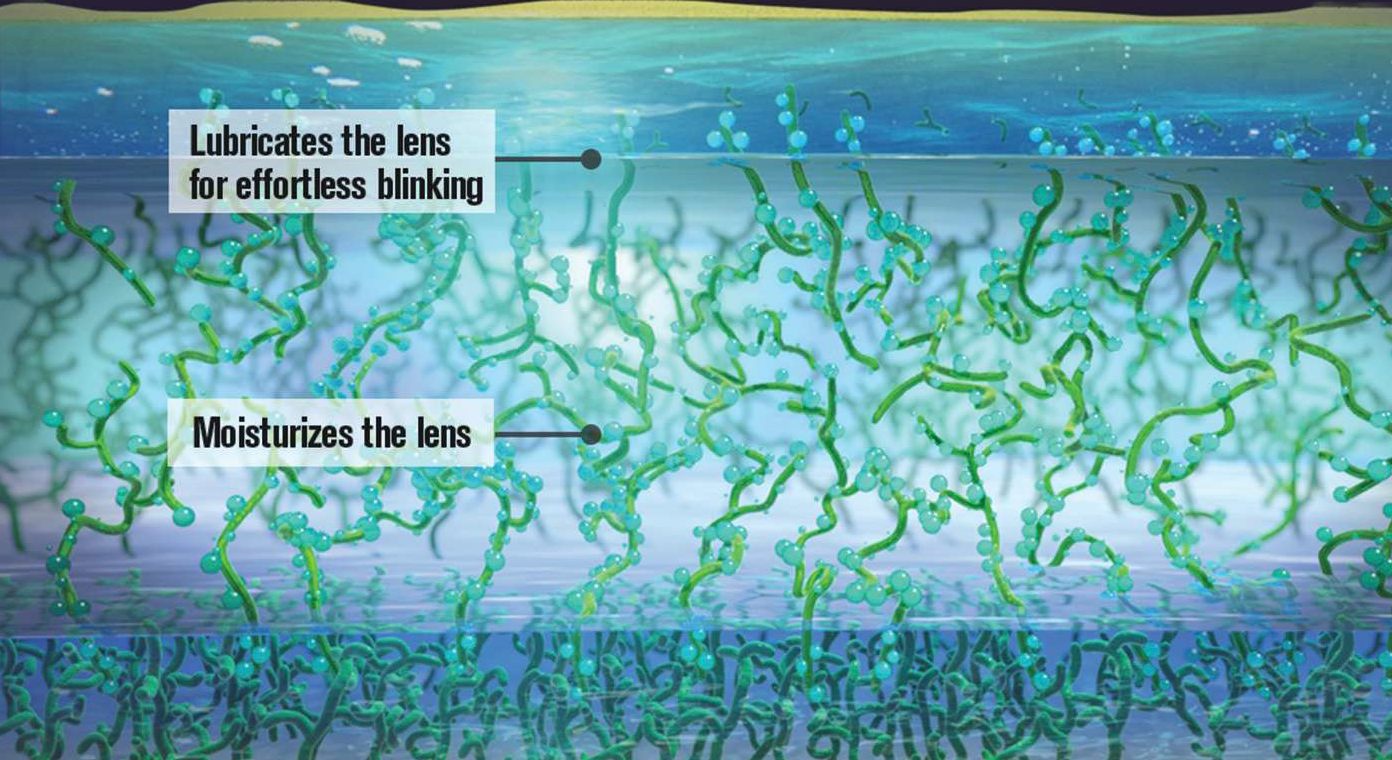
Figure 2: ACUVUE OASYS Brand Contact Lenses 1-Day with HydraLuxe Technology (the middle, lighter section) are comprised of an enhanced network of tear-like molecules plus highly breathable hydrated silicone that integrates with the patient’s own tear film each day.
HOW TO MIMIC MUCINS — AND WHY
At the heart of HydraLuxe Technology is an enhanced moisture network with increased covalent bonding designed to further reduce the adhesiveness of the lens to better mimic the eye’s own mucins. Distributed evenly throughout the enhanced moisture network is high molecular weight polyvinyl pyrrolidone (PVP), a remarkable wetting agent with a long history of use in ophthalmics and biomaterials.9
In HydraLuxe Technology, PVP with a specifically formulated chain length and molecular weight is added to a reactive monomer mix to create a matrix that closely mimics the properties of mucin. Like naturally occurring tear film mucins, the PVP in the lenses contains sites that interact with all key tear components.
Tear-Infused Design
HydraLuxe Technology
• Consists of a uniform tear-like network throughout
the lens (not a coating)
• Works continuously all day (not blink-released)
• Works with key tear components (not just water)
These abilities derive from the amphiphilic nature of PVP that allows it to bind hydrophilic as well as hydrophobic components.
The uniform, nanoscale distribution of PVP throughout the lens allows the material to interact with the ocular environment in such a way that water and tear film components can spread homogenously across and throughout the lens, with minimal heterogeneous precipitation or deposition, so that the lens works with key tear components.10
Recognizing that demanding days require innovative materials and design, ACUVUE OASYS 1-Day with HydraLuxe Technology contact lenses take advantage of the most advanced tear film and contact lens science. The continuous lubrication and moisturizing made possible by precisely formulated PVP combined with the daily disposable modality make these lenses ones that will help keep your patients comfortable throughout their demanding days. OM
REFERENCES
1. Mantelli F, Argüeso P. Functions of ocular surface mucins in health and disease. Curr Opin Allergy Clin Immunol. 2008;8(5):477-83.
2. de Souza GA, Godoy LM, Mann M. Identication of 491 proteins in the tear fluid proteome reveals a large number of proteases and protease inhibitors. Genome Biology. 2006;7(8):R72.
3. Rantamäki AH, Seppänen-Laakso T, Oresic M, et al. Human tear fluid lipidome: from composition to function. PLoS One. 2011;6(5):e19553. doi:10.1371/journal.pone.0019553.
4. Abelson M, Dartt D, McLaughlin J. Mucins: Foundation of A Good Tear Film.Review of Ophthalmology. November 7, 2011. www.reviewofophthalmology.com/content/d/therapeutic_topics/c/30968. Accessed September 2, 2015.
5. Green-Church KB, Butovich I, Willcox M, et al. The International Workshop on Meibomian Gland Dysfunction: Report of the Subcommittee on Tear Film Lipids and Lipid–Protein Interactions in Health and Disease. Invest Ophthalmol Vis Sci. 2011;52(4):1979-93.
6. Definition and Classification of Dry Eye Disease: Report of the definition and classification subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5(2):75-92.
7. Nichols JJ, Willcox MDP, Bron AJ, et al. The TFOS International Workshop on Contact Lens Discomfort: Executive Summary. Invest Ophthalmol Vis Sci. 2013;54:TFOS7-TFOS13.
8. Nichols JJ, Sinnott LT. Tear lm, contact lens, and patient-related factors associated with contact lens-related dry eye. Invest Ophthalmol Vis Sci. 2006;47:1319-28.
9, Polyvinylpyrrolidone. National Library of Medicine. Accessed September 4, 2015: http://toxnet.nlm.nih.gov/cgi-bin/sis/search/a?dbs+hsdb:@term+@DOCNO+205.
10. Oasys patents: US5998498, US6270218, US6367929, US6822016, US6943203, US7461937, US6020445, US6849671, US7052131, US7396890,US7666921, US7691916, US7825170, US8399538, US8450387 D458023, D465416, D496790, D503087, and RE37558.