Points to Remember
- Diabetic eye disease comprises a group of eye conditions that affect people with diabetes. These conditions include diabetic retinopathy, diabetic macular edema (DME), cataract, and glaucoma.
- All forms of diabetic eye disease have the potential to cause severe vision loss and blindness.
- Diabetic retinopathy involves changes to retinal blood vessels that can cause them to bleed or leak fluid, distorting vision.
- Diabetic retinopathy is the most common cause of vision loss among people with diabetes and a leading cause of blindness among working-age adults.
- DME is a consequence of diabetic retinopathy that causes swelling in the area of the retina called the macula.
- Controlling diabetes—by taking medications as prescribed, staying physically active, and maintaining a healthy diet—can prevent or delay vision loss.
- Because diabetic retinopathy often goes unnoticed until vision loss occurs, people with diabetes should get a comprehensive dilated eye exam at least once a year.
- Early detection, timely treatment, and appropriate follow-up care of diabetic eye disease can protect against vision loss.
- Diabetic retinopathy can be treated with several therapies, used alone or in combination.
- NEI supports research to develop new therapies for diabetic retinopathy, and to compare the effectiveness of existing therapies for different patient groups.
What is diabetic eye disease?
Cross section of an eye
Diabetic eye disease can affect many parts of the eye, including the retina, macula, lens and the optic nerve.
Diabetic eye disease is a group of eye conditions that can affect people with diabetes.
- Diabetic retinopathy affects blood vessels in the light-sensitive tissue called the retina that lines the back of the eye. It is the most common cause of vision loss among people with diabetes and the leading cause of vision impairment and blindness among working-age adults.
- Diabetic macular edema (DME). A consequence of diabetic retinopathy, DME is swelling in an area of the retina called the macula.
Diabetic eye disease also includes cataract and glaucoma:
- Cataract is a clouding of the eye’s lens. Adults with diabetes are 2-5 times more likely than those without diabetes to develop cataract. Cataract also tends to develop at an earlier age in people with diabetes.
- Glaucoma is a group of diseases that damage the eye’s optic nerve—the bundle of nerve fibers that connects the eye to the brain. Some types of glaucoma are associated with elevated pressure inside the eye. In adults, diabetes nearly doubles the risk of glaucoma.
All forms of diabetic eye disease have the potential to cause severe vision loss and blindness.
Diabetic Retinopathy
What causes diabetic retinopathy?
Chronically high blood sugar from diabetes is associated with damage to the tiny blood vessels in the retina, leading to diabetic retinopathy. The retina detects light and converts it to signals sent through the optic nerve to the brain. Diabetic retinopathy can cause blood vessels in the retina to leak fluid or hemorrhage (bleed), distorting vision. In its most advanced stage, new abnormal blood vessels proliferate (increase in number) on the surface of the retina, which can lead to scarring and cell loss in the retina.
Diabetic retinopathy may progress through four stages:
Mild nonproliferative retinopathy. Small areas of balloon-like swelling in the retina’s tiny blood vessels, called microaneurysms, occur at this earliest stage of the disease. These microaneurysms may leak fluid into the retina.
Moderate nonproliferative retinopathy. As the disease progresses, blood vessels that nourish the retina may swell and distort. They may also lose their ability to transport blood. Both conditions cause characteristic changes to the appearance of the retina and may contribute to DME.
Severe nonproliferative retinopathy. Many more blood vessels are blocked, depriving blood supply to areas of the retina. These areas secrete growth factors that signal the retina to grow new blood vessels.
Proliferative diabetic retinopathy (PDR). At this advanced stage, growth factors secreted by the retina trigger the proliferation of new blood vessels, which grow along the inside surface of the retina and into the vitreous gel, the fluid that fills the eye. The new blood vessels are fragile, which makes them more likely to leak and bleed. Accompanying scar tissue can contract and cause retinal detachment—the pulling away of the retina from underlying tissue, like wallpaper peeling away from a wall. Retinal detachment can lead to permanent vision loss.
What is diabetic macular edema (DME)?
DME is the build-up of fluid (edema) in a region of the retina called the macula. The macula is important for the sharp, straight-ahead vision that is used for reading, recognizing faces, and driving. DME is the most common cause of vision loss among people with diabetic retinopathy. About half of all people with diabetic retinopathy will develop DME. Although it is more likely to occur as diabetic retinopathy worsens, DME can happen at any stage of the disease.
Who is at risk for diabetic retinopathy?
People with all types of diabetes (type 1, type 2, and gestational) are at risk for diabetic retinopathy. Risk increases the longer a person has diabetes. Between 40 and 45 percent of Americans diagnosed with diabetes have some stage of diabetic retinopathy, although only about half are aware of it. Women who develop or have diabetes during pregnancy may have rapid onset or worsening of diabetic retinopathy.
Symptoms and Detection
What are the symptoms of diabetic retinopathy and DME?
The early stages of diabetic retinopathy usually have no symptoms. The disease often progresses unnoticed until it affects vision. Bleeding from abnormal retinal blood vessels can cause the appearance of “floating” spots. These spots sometimes clear on their own. But without prompt treatment, bleeding often recurs, increasing the risk of permanent vision loss. If DME occurs, it can cause blurred vision.
How are diabetic retinopathy and DME detected?
Diabetic retinopathy and DME are detected during a comprehensive dilated eye exam that includes:
- Visual acuity testing. This eye chart test measures a person’s ability to see at various distances.
- Tonometry. This test measures pressure inside the eye.
- Pupil dilation. Drops placed on the eye’s surface dilate (widen) the pupil, allowing a physician to examine the retina and optic nerve.
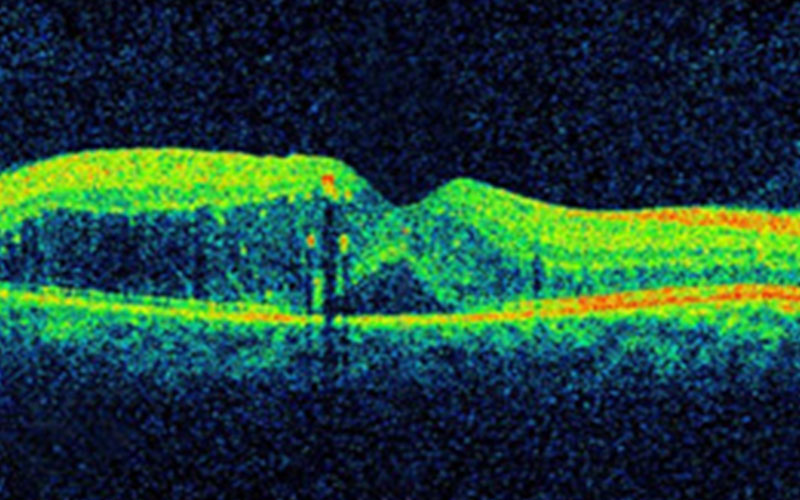
- Optical coherence tomography (OCT). This technique is similar to ultrasound but uses light waves instead of sound waves to capture images of tissues inside the body. OCT provides detailed images of tissues that can be penetrated by light, such as the eye.
A comprehensive dilated eye exam allows the doctor to check the retina for:
- Changes to blood vessels
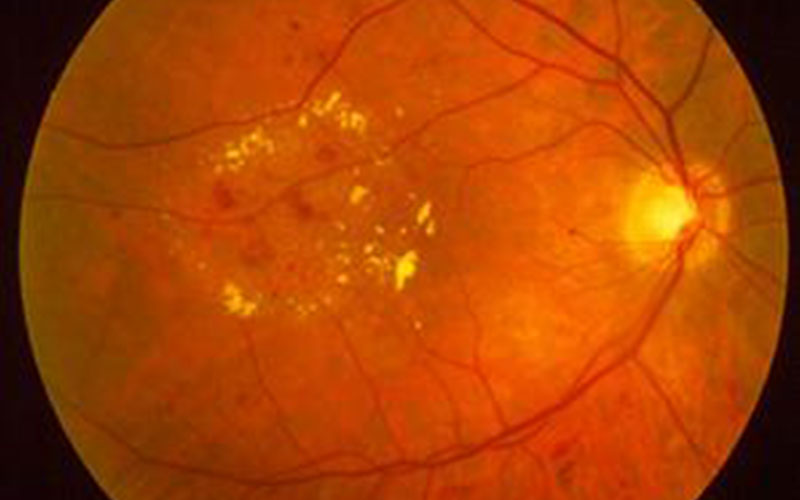
- Leaking blood vessels or warning signs of leaky blood vessels, such as fatty deposits
- Swelling of the macula (DME)
- Changes in the lens
- Damage to nerve tissue
If DME or severe diabetic retinopathy is suspected, a fluorescein angiogram may be used to look for damaged or leaky blood vessels. In this test, a fluorescent dye is injected into the bloodstream, often into an arm vein. Pictures of the retinal blood vessels are taken as the dye reaches the eye.

The same scene as viewed by a person normal vision (left) and with (center) advanced diabetic retinopathy. The floating spots are hemorrhages that require prompt treatment. DME (right) causes blurred vision.
Prevention and Treatment
How can people with diabetes protect their vision?
Vision lost to diabetic retinopathy is sometimes irreversible. However, early detection and treatment can reduce the risk of blindness by 95 percent. Because diabetic retinopathy often lacks early symptoms, people with diabetes should get a comprehensive dilated eye exam at least once a year. People with diabetic retinopathy may need eye exams more frequently. Women with diabetes who become pregnant should have a comprehensive dilated eye exam as soon as possible. Additional exams during pregnancy may be needed.
Studies such as the Diabetes Control and Complications Trial (DCCT) have shown that controlling diabetes slows the onset and worsening of diabetic retinopathy. DCCT study participants who kept their blood glucose level as close to normal as possible were significantly less likely than those without optimal glucose control to develop diabetic retinopathy, as well as kidney and nerve diseases. Other trials have shown that controlling elevated blood pressure and cholesterol can reduce the risk of vision loss among people with diabetes.
Treatment for diabetic retinopathy is often delayed until it starts to progress to PDR, or when DME occurs. Comprehensive dilated eye exams are needed more frequently as diabetic retinopathy becomes more severe. People with severe nonproliferative diabetic retinopathy have a high risk of developing PDR and may need a comprehensive dilated eye exam as often as every 2 to 4 months.
How is DME treated?
DME can be treated with several therapies that may be used alone or in combination.
Anti-VEGF Injection Therapy. Anti-VEGF drugs are injected into the vitreous gel to block a protein called vascular endothelial growth factor (VEGF), which can stimulate abnormal blood vessels to grow and leak fluid. Blocking VEGF can reverse abnormal blood vessel growth and decrease fluid in the retina. Available anti-VEGF drugs include Avastin (bevacizumab), Lucentis (ranibizumab), and Eylea (aflibercept). Lucentis and Eylea are approved by the U.S. Food and Drug Administration (FDA) for treating DME. Avastin was approved by the FDA to treat cancer, but is commonly used to treat eye conditions, including DME.
The NEI-sponsored Diabetic Retinopathy Clinical Research Network compared Avastin, Lucentis, and Eylea in a clinical trial. The study found all three drugs to be safe and effective for treating most people with DME. Patients who started the trial with 20/40 or better vision experienced similar improvements in vision no matter which of the three drugs they were given. However, patients who started the trial with 20/50 or worse vision had greater improvements in vision with Eylea.
Most people require monthly anti-VEGF injections for the first six months of treatment. Thereafter, injections are needed less often: typically three to four during the second six months of treatment, about four during the second year of treatment, two in the third year, one in the fourth year, and none in the fifth year. Dilated eye exams may be needed less often as the disease stabilizes.
Avastin, Lucentis, and Eylea vary in cost and in how often they need to be injected, so patients may wish to discuss these issues with an eye care professional.
Focal/grid macular laser surgery. In focal/grid macular laser surgery, a few to hundreds of small laser burns are made to leaking blood vessels in areas of edema near the center of the macula. Laser burns for DME slow the leakage of fluid, reducing swelling in the retina. The procedure is usually completed in one session, but some people may need more than one treatment. Focal/grid laser is sometimes applied before anti-VEGF injections, sometimes on the same day or a few days after an anti-VEGF injection, and sometimes only when DME fails to improve adequately after six months of anti-VEGF therapy.
Corticosteroids. Corticosteroids, either injected or implanted into the eye, may be used alone or in combination with other drugs or laser surgery to treat DME. The Ozurdex (dexamethasone) implant is for short-term use, while the Iluvien (fluocinolone acetonide) implant is longer lasting. Both are biodegradable and release a sustained dose of corticosteroids to suppress DME. Corticosteroid use in the eye increases the risk of cataract and glaucoma. DME patients who use corticosteroids should be monitored for increased pressure in the eye and glaucoma.
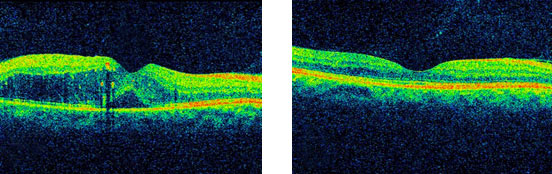
The retina of a person with diabetic retinopathy and DME, as viewed by optical coherence tomography (OCT). The two images were taken before (left) and after anti-VEGF treatment (right). The dip in the retina is the fovea, a region of the macula where vision is normally at its sharpest. Note the swelling of the macula and elevation of the fovea before treatment.
How is proliferative diabetic retinopathy (PDR) treated?
For decades, PDR has been treated with scatter laser surgery, sometimes called panretinal laser surgery or panretinal photocoagulation. Treatment involves making 1,000 to 2,000 tiny laser burns in areas of the retina away from the macula. These laser burns are intended to cause abnormal blood vessels to shrink. Although treatment can be completed in one session, two or more sessions are sometimes required. While it can preserve central vision, scatter laser surgery may cause some loss of side (peripheral), color, and night vision. Scatter laser surgery works best before new, fragile blood vessels have started to bleed. Recent studies have shown that anti-VEGF treatment not only is effective for treating DME, but is also effective for slowing progression of diabetic retinopathy, including PDR, so anti-VEGF is increasingly used as a first-line treatment for PDR.
What is a vitrectomy?
A vitrectomy is the surgical removal of the vitreous gel in the center of the eye. The procedure is used to treat severe bleeding into the vitreous, and is performed under local or general anesthesia. Ports (temporary water-tight openings) are placed in the eye to allow the surgeon to insert and remove instruments, such as a tiny light or a small vacuum called a vitrector. A clear salt solution is gently pumped into the eye through one of the ports to maintain eye pressure during surgery and to replace the removed vitreous. The same instruments used during vitrectomy also may be used to remove scar tissue or to repair a detached retina.
Vitrectomy may be performed as an outpatient procedure or as an inpatient procedure, usually requiring a single overnight stay in the hospital. After treatment, the eye may be covered with a patch for days to weeks and may be red and sore. Drops may be applied to the eye to reduce inflammation and the risk of infection. If both eyes require vitrectomy, the second eye usually will be treated after the first eye has recovered.
What if treatment doesn’t improve vision?
An eye care professional can help locate and make referrals to low vision and rehabilitation services and suggest devices that may help make the most of remaining vision. Many community organizations and agencies offer information about low vision counseling, training, and other special services for people with visual impairment. A nearby school of medicine or optometry also may provide low vision and rehabilitation services.
Current Research
What is the NEI doing to advance research on diabetic eye disease?
The NEI is conducting and supporting research that seeks better ways to detect, treat, and prevent vision loss in people with diabetes. This research is being conducted in labs and clinical centers across the country.
For example, the Diabetic Retinopathy Clinical Research Network (DRCR.net) conducts large multi-center trials to test new therapies for diabetic eye disease, and to compare different therapies. The network formed in 2002 and comprises more than 350 physicians practicing at more than 140 clinical sites across the country. Many of the sites are private practice eye clinics, enabling the network to quickly bring innovative treatments from research into community practice.
NEI-funded scientists are also seeking ways to detect diabetic retinopathy at earlier stages. For example, researchers are harnessing a technology called adaptive optics (AO) to improve imaging techniques such as OCT. AO was developed by astronomers seeking to improve the resolution of their telescopes by filtering out distortions in the atmosphere. In the clinic, diagnostic devices that use AO may improve the detection of subtle changes in retinal tissue and blood vessels.
The National Eye Institute (NEI) is part of the National Institutes of Health (NIH) and is the Federal government’s lead agency for vision research that leads to sight-saving treatments and plays a key role in reducing visual impairment and blindness.
Last Reviewed: September 2015